The Role of Nutrition in Dementia
Nutrition plays a significant role in maintaining overall health, and for individuals living with dementia, it becomes even more crucial. As cognitive function declines, the body’s nutritional needs may change, and eating habits can be affected. Poor nutrition can exacerbate symptoms like confusion, fatigue, and mood changes, while a well-balanced diet can help support brain function and general well-being. The goal is not to cure dementia through diet but to help manage symptoms and improve quality of life through thoughtful nutrition choices.
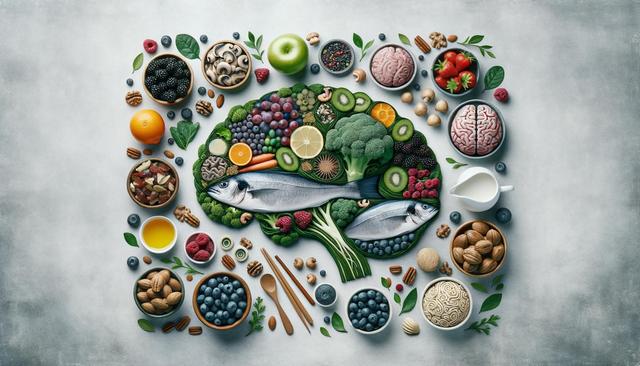
Several studies suggest that diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can be beneficial for brain health. These foods provide essential nutrients such as antioxidants, vitamins, and omega-3 fatty acids that may help reduce inflammation and oxidative stress, both of which are linked to cognitive decline. Tailoring a diet plan to the individual’s preferences, cultural habits, and medical conditions is essential for long-term adherence and effectiveness.
Key Nutrients and Foods to Include
Focusing on nutrient-dense foods can help support cognitive function and overall health. Some nutrients have been specifically studied for their potential benefits in dementia care. These include:
- Omega-3 fatty acids: Found in fatty fish, flaxseeds, and walnuts, these may support brain cell structure and function.
- Antioxidants: Berries, dark leafy greens, and colorful vegetables are rich in antioxidants that help protect brain cells from damage.
- B vitamins: Especially B6, B12, and folate, found in whole grains, legumes, and animal products, which help in maintaining healthy nerve function.
- Vitamin D: Supports brain and bone health and can be obtained through fortified foods and controlled sun exposure.
Including these nutrients regularly in meals can be helpful, but it’s also critical to balance intake with the individual’s specific health needs, such as diabetes, cardiovascular disease, or swallowing difficulties.
Challenges in Eating and Appetite
Dementia often affects a person’s ability to eat safely and consistently. Changes in taste, forgetfulness about meals, or difficulty using utensils can make eating a challenge. In some cases, individuals may develop preferences for sweet or salty foods or may forget that they’ve already eaten. Caregivers should be mindful of these changes and prepare meals that are both nutritious and easy to manage.
Practical tips for overcoming eating challenges include:
- Serving smaller, more frequent meals
- Offering finger foods for easier handling
- Using contrasting plate colors to help distinguish food
- Creating a calm and distraction-free eating environment
Monitoring hydration is equally important, as individuals with dementia may forget to drink water regularly. Offering fluids throughout the day, including soups and water-rich fruits, can help prevent dehydration.
Dietary Patterns That May Support Brain Health
Some dietary patterns have been associated with better brain health and may be helpful in the context of dementia care. While these eating patterns are not cures, they provide a framework for building a brain-friendly diet. Two commonly referenced approaches include:
- Mediterranean diet: Emphasizes vegetables, fruits, whole grains, legumes, fish, and healthy fats like olive oil.
- MIND diet: A combination of the Mediterranean and DASH diets, with a focus on foods thought to reduce the risk of cognitive decline.
These diets encourage the consumption of foods that are low in saturated fat and high in nutrients. They also recommend limiting red meat, processed foods, and sugary snacks. For individuals with dementia, these diets can be adapted to meet personal preferences while emphasizing variety and nutrient density.
Creating meal plans based on these dietary frameworks can offer structure and consistency, making it easier for caregivers to ensure nutritional needs are met.
Practical Meal Planning and Support
When planning meals for someone with dementia, simplicity and nutrition should go hand in hand. Meals should be easy to prepare, visually appealing, and tailored to the individual’s eating abilities and preferences. Involving the person with dementia in meal planning, shopping, or preparation—if feasible—can increase engagement and appetite.
Some practical meal planning tips include:
- Preparing meals in advance and storing them in labeled containers
- Keeping a regular meal schedule to build routine
- Using familiar foods to encourage eating
- Monitoring for food sensitivities or changes in tolerance
In some cases, nutritional supplements may be considered if intake is insufficient, but these should only be used under medical guidance. Caregivers should also be alert to signs of malnutrition or unintended weight loss and seek advice from a healthcare provider or registered dietitian when necessary.
Support groups and community resources can be valuable for caregivers navigating the challenges of dementia and nutrition. Sharing experiences and tips with others in similar situations can provide emotional support and practical advice.
Conclusion: Supporting Brain Health Through Thoughtful Nutrition
Nutrition is a powerful tool in the care and support of individuals with dementia. While it cannot reverse the condition, a well-considered diet can help improve quality of life, manage symptoms, and support overall health. Caregivers play a vital role in ensuring that meals are not only nutritious but also accessible and enjoyable. By focusing on balanced, nutrient-rich foods and overcoming eating challenges with empathy and creativity, caregivers can make a meaningful difference in the daily lives of those living with dementia.