Understanding Bariatric Surgery and Its Purpose
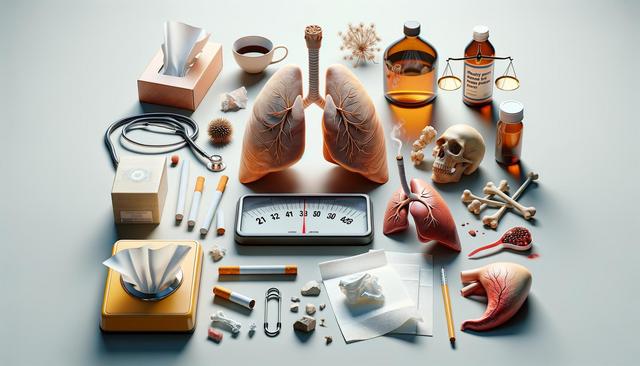
Bariatric surgery refers to various procedures designed to assist individuals with significant weight loss when traditional methods like diet and exercise have not been effective. These surgical interventions alter the digestive system to limit food intake or reduce nutrient absorption, ultimately leading to weight loss. While there are several types of bariatric surgery, including gastric bypass, sleeve gastrectomy, and adjustable gastric banding, each has the common goal of helping patients achieve a healthier weight and reduce the risks of obesity-related conditions.
This type of surgery is generally recommended for individuals with a body mass index (BMI) of 40 or higher, or a BMI of 35 or more with at least one serious health issue linked to obesity, such as type 2 diabetes, hypertension, or sleep apnea. The decision to undergo bariatric surgery is a major one and usually follows thorough discussions with healthcare providers, nutritional experts, and sometimes mental health professionals. These evaluations help determine whether the procedure is a suitable and safe option for the patient.
Types of Bariatric Surgery Procedures
There are several common types of bariatric surgery, each with its own approach and benefits. Understanding the differences can help patients and their healthcare teams make informed choices regarding which procedure aligns best with their health goals and circumstances.
- Sleeve Gastrectomy: This involves removing a large portion of the stomach, leaving a small, banana-shaped section. It reduces hunger and limits how much food can be consumed.
- Roux-en-Y Gastric Bypass: This procedure creates a small pouch at the top of the stomach and connects it directly to the small intestine, bypassing a large portion of the stomach and duodenum.
- Adjustable Gastric Band: A band is placed around the upper part of the stomach to form a small pouch that limits food intake. The band is adjustable and can be tightened or loosened over time.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): This is a less common but highly complex surgery that includes both restriction and malabsorption components.
Each procedure has unique advantages and potential drawbacks, and the choice often depends on the patient’s weight, health history, and long-term goals.
What to Expect Before Surgery
Preparing for bariatric surgery involves more than just scheduling the operation. Patients undergo a comprehensive evaluation that includes physical exams, lab testing, nutritional counseling, and mental health assessments. These steps ensure the patient is physically and emotionally ready for the changes that come with surgery.
Pre-surgery preparation may also include:
- A medically supervised weight loss program
- Smoking cessation if applicable
- Adjusting current medications
- Meeting with a dietitian to understand post-surgery nutritional needs
Patients are typically advised to follow a specific pre-operative diet to reduce the size of the liver, which makes the surgery safer and more effective. This diet often consists of high-protein, low-carbohydrate meals and may include meal replacements. Setting realistic expectations and understanding the commitment required for long-term success is crucial at this stage.
Post-Surgery Recovery and Lifestyle Changes
Recovery from bariatric surgery varies depending on the type of procedure and the individual’s health. Most patients stay in the hospital for one to three days, with full recovery taking several weeks. During this time, patients gradually transition from a liquid diet to pureed foods, and eventually to solid meals, under the guidance of a healthcare provider or dietitian.
Key lifestyle changes after surgery include:
- Eating smaller, more frequent meals
- Chewing food thoroughly and eating slowly
- Staying hydrated, but not drinking fluids with meals
- Taking prescribed vitamin and mineral supplements daily
- Incorporating regular physical activity
These adjustments help prevent complications such as dumping syndrome, nutritional deficiencies, or weight regain. Many patients also attend support groups or counseling sessions to help navigate the emotional and psychological aspects of post-surgery life.
Long-Term Results and Considerations
While bariatric surgery can lead to significant and sustained weight loss, long-term success depends heavily on a patient’s commitment to lifestyle changes. Studies have shown that many individuals maintain weight loss for years, and many health conditions improve or resolve following surgery, such as type 2 diabetes, high blood pressure, and joint pain.
However, it’s important to note that:
- Weight loss may plateau or fluctuate over time
- Ongoing follow-up care is essential to monitor nutritional health
- Psychological support may be needed to manage body image or eating habits
- Some patients may require additional procedures or interventions
Maintaining a structured routine that includes healthy eating, regular exercise, and medical checkups helps reinforce positive outcomes. Furthermore, staying informed and engaged with a supportive healthcare team can make a significant difference in sustaining the benefits of bariatric surgery.