Understanding Stage 3 Chronic Kidney Disease
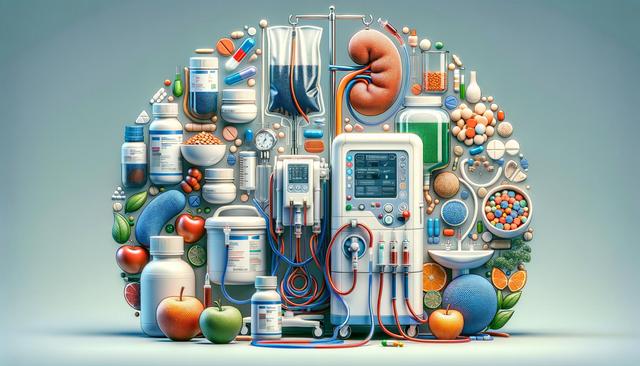
Stage 3 chronic kidney disease (CKD) is characterized by a moderate decline in kidney function, typically with an estimated glomerular filtration rate (eGFR) between 30 and 59 mL/min. At this stage, many people may not experience noticeable symptoms, but it’s a critical time to begin interventions that can preserve kidney function and prevent further decline. Early identification and consistent monitoring are essential. Regular lab tests to track eGFR, creatinine levels, and urine protein are typically ordered to monitor disease progression.
CKD stage 3 is often divided into two sub-stages: 3a (eGFR 45–59) and 3b (eGFR 30–44). While both indicate moderate kidney function loss, individuals in stage 3b may be at a higher risk for complications. These include cardiovascular issues, anemia, and mineral and bone disorders. Understanding the nuances of stage 3 CKD helps healthcare providers tailor treatment strategies more effectively.
Dietary Adjustments and Nutritional Support
One of the most impactful lifestyle changes for managing CKD stage 3 is adopting a kidney-friendly diet. Nutrition plays a vital role in reducing the kidneys’ workload and controlling the buildup of waste in the blood. Working with a registered dietitian familiar with kidney disease is highly recommended to create a personalized meal plan.
Key dietary recommendations may include:
- Reducing sodium intake to help manage blood pressure and reduce fluid retention
- Limiting protein consumption to decrease waste buildup while maintaining muscle mass
- Controlling potassium and phosphorus levels to prevent complications like heart rhythm disturbances and bone issues
- Staying adequately hydrated without overloading the kidneys
In addition to these adjustments, patients should pay close attention to food labels and portion sizes. Monitoring nutrient intake can help prevent the progression of CKD and improve overall well-being.
Medical Treatment and Medication Management
Pharmacological treatment plays an essential role in managing CKD stage 3. The goal is to control underlying conditions and reduce kidney stress. Common medical interventions include medications for high blood pressure, diabetes, and cholesterol—all of which can affect kidney health.
Commonly prescribed medications may include:
- ACE inhibitors or ARBs to manage blood pressure and reduce protein in urine
- Statins to manage cholesterol levels
- Phosphate binders for those with high phosphorus levels
- Iron supplements or erythropoiesis-stimulating agents for anemia
It’s crucial for patients to review all medications with their healthcare provider, including over-the-counter drugs and supplements, to avoid nephrotoxic substances. Medication adherence and regular follow-ups significantly contribute to slowing CKD progression.
Lifestyle Modifications for Kidney Health
Beyond diet and medication, lifestyle habits have a profound effect on kidney health. Making sustainable, healthy changes can support kidney function and improve quality of life. Individuals with CKD stage 3 are encouraged to adopt habits that reduce the risk of complications and support overall wellness.
Helpful lifestyle strategies include:
- Engaging in regular physical activity, such as walking or light aerobic exercise
- Maintaining a healthy weight to reduce strain on the kidneys
- Quitting smoking, which can accelerate the decline in kidney function
- Managing stress through mindfulness practices or counseling
These strategies not only help protect kidney function but also contribute to cardiovascular health, which is closely linked to kidney outcomes. Incremental changes, when consistently practiced, can lead to significant long-term benefits.
Monitoring and Collaborative Care
Managing CKD stage 3 effectively requires ongoing monitoring and a team-based approach. Regular visits with a primary care physician, nephrologist, and other specialists ensure that any changes in health status are promptly addressed. Coordinated care also helps manage comorbidities that commonly accompany CKD, such as diabetes and hypertension.
Key components of ongoing monitoring include:
- Routine blood and urine tests to assess kidney function and electrolyte balance
- Blood pressure monitoring at home and during clinic visits
- Evaluation of bone health and anemia-related markers
- Timely imaging tests, when necessary, to evaluate kidney structure
Collaboration between healthcare providers and patients is critical. Patients are encouraged to stay informed about their condition, ask questions, and actively participate in their care plan. Educational resources, support groups, and digital tools can also enhance self-management.