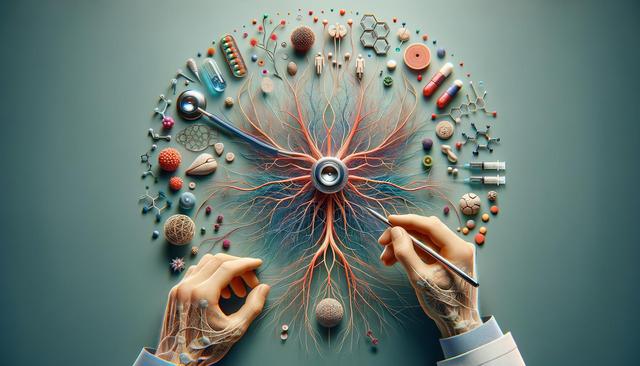
Understanding Peripheral Neuropathy and Its Causes
Peripheral neuropathy refers to a condition that results from damage to the peripheral nerves, which are responsible for sending signals between the central nervous system and the rest of the body. This damage can lead to a range of symptoms such as tingling, burning sensations, muscle weakness, and even sensory loss. There are over 100 types of peripheral neuropathy, and they can develop from various underlying causes. The most common include diabetes, infections, inherited disorders, exposure to toxins, and physical trauma. In some cases, the exact cause remains unknown, which can complicate treatment.
Identifying the root cause is essential in managing and treating peripheral neuropathy effectively. Accurate diagnosis often involves a combination of medical history review, neurological exams, blood tests, imaging studies, and nerve conduction tests. Understanding the origin of the nerve damage allows healthcare professionals to tailor treatment strategies to address the specific needs of each patient.
Medications and Pharmacological Interventions
For many individuals, medications are a key part of managing peripheral neuropathy symptoms. While they may not reverse nerve damage, they can help reduce pain and improve quality of life. Commonly prescribed drugs for neuropathy include:
- Antidepressants, particularly tricyclic antidepressants and serotonin-norepinephrine reuptake inhibitors (SNRIs), which help modify pain signals in the brain.
- Anticonvulsants, such as gabapentin and pregabalin, which are originally used for epilepsy but have shown efficacy in managing nerve pain.
- Topical treatments, like capsaicin cream or lidocaine patches, can provide localized relief for mild to moderate pain.
- Pain relievers, including over-the-counter options like acetaminophen and ibuprofen, though stronger painkillers may be prescribed for severe cases.
It’s important to work closely with a healthcare provider to monitor the effectiveness of these medications and adjust dosages as needed. Side effects and potential interactions with other drugs should also be considered when beginning any pharmacological treatment.
Lifestyle Adjustments and Self-Care Strategies
In addition to medication, lifestyle changes can significantly impact the management of peripheral neuropathy. These adjustments often support overall health and may help slow the progression of nerve damage. Some effective self-care strategies include:
- Regular physical activity, such as walking or swimming, to improve circulation and reduce discomfort.
- Maintaining a balanced diet rich in vitamins and minerals, especially B vitamins that are essential for nerve health.
- Quitting smoking and reducing alcohol intake, both of which can aggravate nerve damage.
- Practicing good foot care, particularly for individuals with diabetes, to prevent injuries that may go unnoticed due to numbness.
Stress management techniques like yoga, meditation, and deep breathing exercises can also help manage chronic pain and improve emotional well-being. These lifestyle modifications aim to create a holistic approach to managing the condition.
Physical Therapy and Alternative Treatments
Physical therapy can be highly beneficial for individuals with peripheral neuropathy, especially when the condition affects mobility and balance. Therapists can design personalized exercise programs to strengthen muscles, improve coordination, and reduce the risk of falls. Occupational therapy may also be recommended to help patients adapt their daily activities and maintain independence.
Some patients find relief through complementary and alternative treatments. These may include:
- Acupuncture, which may stimulate nerves and enhance blood flow.
- Massage therapy, which can alleviate tension and promote relaxation.
- Transcutaneous electrical nerve stimulation (TENS), a technique that uses low-voltage electrical currents to relieve pain.
While the effectiveness of these methods can vary from person to person, they are generally considered safe when performed by qualified professionals. It’s wise to discuss any alternative treatments with a healthcare provider to ensure they align with the overall treatment plan.
Emerging and Advanced Therapies
Ongoing research continues to explore new ways to treat peripheral neuropathy. Some of the more recent and innovative therapies show promising results, although many are still in experimental stages. Among these are:
- Regenerative medicine approaches, including stem cell therapy, aimed at repairing or replacing damaged nerve tissues.
- Gene therapy, which may target the genetic components of inherited neuropathies.
- Neurostimulation devices, such as spinal cord stimulators, which can help modulate pain signals directly.
In addition to these, clinical trials are actively testing novel medications and interventions that could lead to more effective treatments in the future. Patients interested in these options should consult with a specialist or research institution to determine eligibility and potential benefits.
Access to these emerging treatments may be limited, and not all are covered by insurance. Therefore, it’s important for patients to consider both the potential outcomes and the practical aspects, including cost and availability, when exploring advanced therapies.
Conclusion: Taking a Comprehensive Approach to Treatment
Managing peripheral neuropathy requires a multifaceted approach that considers the underlying cause, symptom severity, and individual patient needs. From medications and physical therapy to lifestyle changes and emerging therapies, a wide range of treatment options are available. While no single treatment works for everyone, combining several strategies often yields the most effective results.
For individuals living with peripheral neuropathy, staying informed and proactive can make a meaningful difference. Regular communication with healthcare providers, open-mindedness to new therapies, and commitment to self-care are all important aspects of long-term management. With the right support and resources, many people can find relief from their symptoms and maintain a fulfilling quality of life.