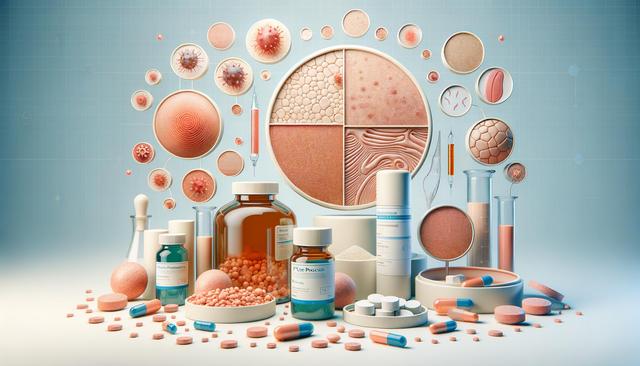
What Is Plaque Psoriasis?
Plaque psoriasis is a chronic autoimmune condition that primarily affects the skin, leading to the development of raised, red patches covered with a silvery-white buildup of dead skin cells. These patches, or plaques, commonly appear on the elbows, knees, scalp, and lower back, although they can develop anywhere on the body. The disease tends to follow a cycle, flaring for a few weeks or months and then subsiding or going into remission. While the exact cause of plaque psoriasis is not entirely known, it is understood to be related to an overactive immune system that speeds up the lifecycle of skin cells.
Plaque psoriasis is not contagious, but it can have a significant impact on a person’s quality of life, both physically and emotionally. In addition to the visible skin symptoms, individuals may also experience itching, burning, and soreness in the affected areas. The condition can also be linked to other health issues, including psoriatic arthritis, cardiovascular disease, and depression. Understanding the nature of plaque psoriasis is the first step in managing its symptoms and seeking appropriate treatment.
Recognizing the Symptoms
The symptoms of plaque psoriasis can vary in severity from one person to another. However, some common signs are shared among most individuals who suffer from this condition. The hallmark feature is the presence of thickened, red skin that is often covered with silvery-white scales. These plaques are typically itchy, and in some cases, they may crack and bleed. Other symptoms may include:
- Dry, cracked skin that may bleed
- Burning or soreness around the patches
- Thickened or ridged nails
- Scalp scaling similar to dandruff
In more severe cases, plaque psoriasis can affect large portions of the body and may be accompanied by joint pain—an indication of psoriatic arthritis. Flare-ups can be triggered by various factors including stress, infections, skin injuries, certain medications, and changes in weather. Tracking these triggers can help manage symptoms more effectively and reduce future outbreaks.
Medication Options for Treatment
There are several types of medications available to manage plaque psoriasis, and the choice of treatment often depends on the severity of symptoms and the patient’s overall health. Topical treatments are commonly used for mild to moderate cases and include corticosteroids, vitamin D analogs, and salicylic acid. These are applied directly to the skin to reduce inflammation and slow down the growth of skin cells.
For more extensive or resistant cases, systemic medications may be necessary. These include:
- Oral medications that affect the immune system
- Biologic drugs administered by injection or infusion
- Phototherapy using ultraviolet light
Biologics are among the newer treatment options and are designed to target specific parts of the immune system. They are often used when other treatments have not been effective. However, like all medications, they come with potential side effects and risks, which should be discussed with a healthcare provider. Monitoring is essential to ensure that the benefits outweigh any possible adverse effects.
Non-Medication Approaches and Lifestyle Considerations
While medications play a crucial role in managing plaque psoriasis, non-medication approaches can also be highly beneficial. Lifestyle changes and self-care routines can help reduce symptoms and improve overall well-being. Some effective strategies include:
- Using moisturizers regularly to prevent dryness and scaling
- Taking lukewarm baths with added bath oils or colloidal oatmeal
- Avoiding known triggers such as stress and smoking
- Maintaining a healthy diet and body weight
Stress management techniques such as yoga, meditation, and regular exercise can also contribute to fewer flare-ups. For some individuals, dietary changes—such as reducing alcohol intake and avoiding inflammatory foods—may help. It’s important to note that while these methods may not replace medical treatments, they can significantly enhance their effectiveness and help control the condition over time.
Support groups and counseling can also be valuable resources, especially for those dealing with the emotional aspects of plaque psoriasis. Feeling supported and informed can make a meaningful difference in managing a chronic condition like this.
When to See a Healthcare Provider
Because plaque psoriasis is a chronic condition, ongoing medical care is often necessary. It is advisable to consult a healthcare provider if you suspect you have psoriasis or if your current treatment is no longer effective. Early diagnosis and intervention can prevent the condition from worsening and reduce the risk of associated health complications.
Some signs that indicate a visit to a healthcare provider is necessary include:
- Rapid worsening of symptoms
- Development of joint pain or stiffness
- Side effects from medications
- Emotional distress related to the condition
Doctors may perform a physical examination and, in some cases, a skin biopsy to confirm the diagnosis. They can then recommend an appropriate treatment plan tailored to your needs. Regular follow-ups are important to monitor progress and make any necessary adjustments to therapy. Don’t hesitate to seek a second opinion if you feel your concerns are not being addressed.
Managing plaque psoriasis effectively involves a partnership between the patient and healthcare provider. With a combination of the right treatments, lifestyle adjustments, and ongoing support, many people are able to maintain control over their symptoms and lead fulfilling lives.
Conclusion: Taking Control of Plaque Psoriasis
Plaque psoriasis is a manageable skin condition, although it can present ongoing challenges. Recognizing the symptoms early, exploring various treatment options, and making supportive lifestyle changes can significantly improve quality of life. Whether the condition is mild or more severe, staying informed and proactive is key. Regular communication with healthcare professionals and a commitment to personal well-being can help keep symptoms under control and reduce the impact of flare-ups. By understanding the range of available treatments and integrating healthy habits, individuals can take meaningful steps toward managing plaque psoriasis effectively.