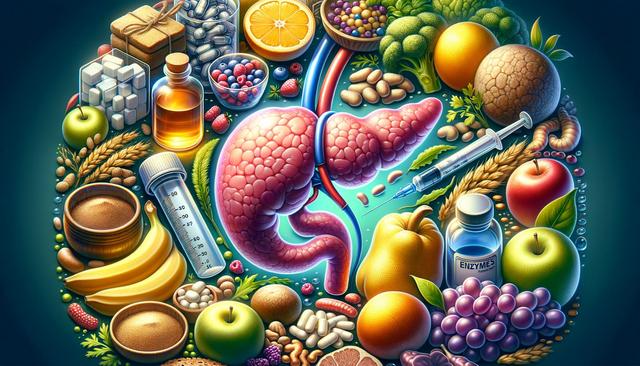
What Is Pancreatitis and Why It Happens
Pancreatitis is an inflammation of the pancreas, a vital organ that helps digest food and regulate blood sugar. This condition can be acute, developing suddenly and lasting for a few days, or chronic, persisting over many years. It typically occurs when digestive enzymes become active inside the pancreas instead of the small intestine, leading to irritation and damage. Common causes include gallstones, heavy alcohol use, certain medications, and high levels of triglycerides in the blood. Recognizing early signs and understanding the triggers is crucial for managing the condition effectively.
People with pancreatitis often experience upper abdominal pain that may radiate to the back, nausea, vomiting, fever, and a tender abdomen. Chronic pancreatitis may lead to weight loss and oily, foul-smelling stools due to poor nutrient absorption. Without proper care, chronic inflammation can lead to permanent damage or complications such as diabetes and digestive issues. Early diagnosis and lifestyle adjustments are key to long-term management.
The Role of Enzymes in Treating Pancreatitis
When the pancreas is inflamed or damaged, it may not produce enough enzymes to break down food properly. In such cases, doctors may recommend enzyme replacement therapy to support digestion and reduce pancreatic workload. These enzymes are usually taken in capsule form with meals and snacks to help the body absorb nutrients. The supplements typically include lipase, protease, and amylase, which help digest fats, proteins, and carbohydrates respectively.
Enzyme therapy can improve symptoms like bloating, gas, and stool irregularities. It also aids in maintaining a healthy weight and ensuring that the body receives essential nutrients. However, it’s important for individuals to follow the prescribed dosage and timing instructions carefully. Self-medicating or using over-the-counter enzymes without medical advice is not recommended, as incorrect use may worsen symptoms or cause other issues.
In addition to enzymes, treatment may include pain relief, hydration, and dietary changes. Enzymes are not a cure, but they play a supportive role in managing chronic pancreatitis and improving quality of life.
Recognizing the Signs of Pancreatitis
Knowing the signs of pancreatitis can help individuals seek timely medical attention. The symptoms may vary depending on whether the condition is acute or chronic. Some common signs include:
- Severe abdominal pain that may worsen after eating
- Nausea and vomiting
- Fever and rapid pulse
- Swollen or tender abdomen
- Unexplained weight loss
- Greasy or pale stools
In severe cases, pancreatitis may lead to complications such as internal bleeding, infection, or organ failure. Chronic pancreatitis may also affect insulin production, leading to diabetes. If any of these signs are noticed, it is essential to consult a healthcare provider for proper diagnosis and treatment. Blood tests, imaging scans, and stool analyses are commonly used to confirm the condition and determine its severity.
Timely recognition and ongoing monitoring are essential to prevent the progression of pancreatitis and reduce the risk of long-term complications.
Foods to Avoid with Pancreatitis
Diet plays a major role in managing pancreatitis. Certain foods can trigger or worsen inflammation, so it’s important to make thoughtful dietary choices. A low-fat, nutrient-rich diet is often recommended, along with avoiding alcohol and processed foods. Here are some foods that should generally be avoided:
- Fried and greasy foods such as chips, bacon, and fast food
- Butter, cream, and full-fat dairy products
- Red meat and high-fat cuts of pork
- Pastries, cakes, and sugary desserts
- Alcoholic beverages
- Spicy or heavily seasoned foods
Instead, individuals are encouraged to eat foods that are easier to digest and less taxing on the pancreas. These include lean proteins, steamed vegetables, whole grains, and non-fat dairy options. Drinking plenty of water and eating smaller, frequent meals can also help manage symptoms. In some cases, a registered dietitian may provide a personalized meal plan to ensure nutritional needs are met while reducing flare-ups.
By avoiding certain trigger foods and focusing on gut-friendly nutrition, individuals with pancreatitis can support their healing process and enhance treatment outcomes.
Long-Term Care and Lifestyle Adjustments
Managing pancreatitis requires more than just medical treatment. Long-term care involves lifestyle modifications that support pancreatic health and reduce the likelihood of flare-ups. These changes often include:
- Quitting alcohol and smoking completely
- Maintaining a healthy, low-fat diet
- Staying hydrated and managing stress
- Following prescribed medications and enzyme therapy
- Regular medical check-ups to monitor progress
Patients may also benefit from joining support groups or speaking with a counselor to cope with the emotional aspects of living with a chronic condition. Chronic pancreatitis can have a significant impact on quality of life, but with the right care plan and support, many individuals can lead active and fulfilling lives. Monitoring blood sugar levels and nutritional intake is also essential, especially if diabetes develops as a complication.
In some cases, surgery or procedures to remove blockages, drain cysts, or address complications may be necessary. However, with early intervention and consistent care, many people can manage their symptoms and reduce hospital visits over time.
Conclusion: Supporting Recovery with Knowledge and Care
Pancreatitis is a serious condition that requires attention, but with proper knowledge and action, it can be effectively managed. Understanding the role of enzymes, recognizing warning signs, avoiding harmful foods, and making lasting lifestyle changes are all vital steps toward recovery. For those affected, working closely with healthcare providers and maintaining a supportive routine can make a significant difference in overall well-being and long-term health.